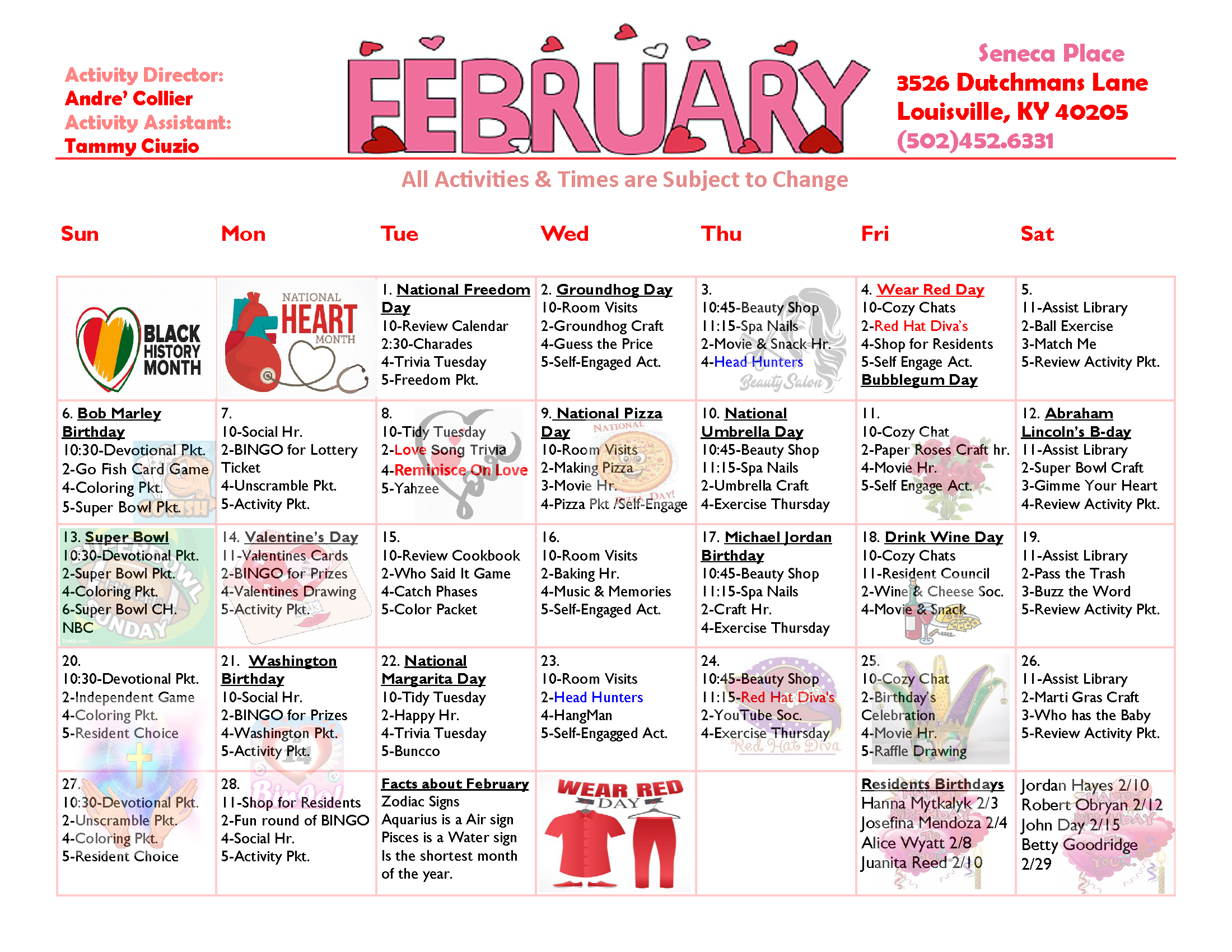
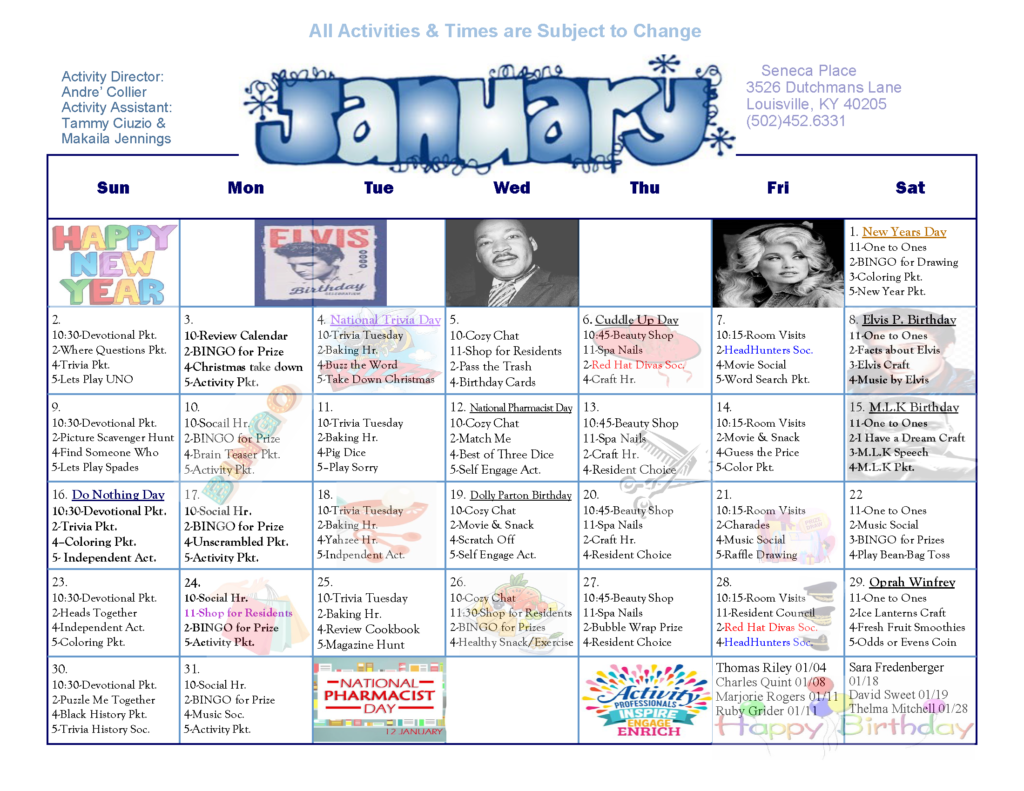
Heart Health and Aging
July 22, 2024HOW DOES THE HEART WORK?
Your heart is a strong muscle that pumps blood to your body. A normal, healthy adult heart is about the size of your clenched fist. Just like an engine makes a car go, the heart keeps your body running. The heart has two sides, each with a top chamber (atrium) and a bottom chamber (ventricle). The right side pumps blood to the lungs to pick up oxygen. The left side receives blood rich with oxygen from the lungs and pumps it through arteries throughout the body. An electrical system in the heart controls the heart rate (heartbeat or pulse) and coordinates the contraction of the heart’s top and bottom chambers.
HOW YOUR HEART CHANGES WITH AGE
People age 65 and older are much more likely than younger people to suffer a heart attack, to have a stroke, or to develop coronary heart disease (commonly called heart disease) and heart failure. Heart disease is also a major cause of disability, limiting the activity and eroding the quality of life of millions of older people.
Aging can cause changes in the heart and blood vessels. For example, as you get older, your heart can’t beat as fast during physical activity or times of stress as it did when you were younger. However, the number of heartbeats per minute (heart rate) at rest does not change significantly with normal aging.
Changes that happen with age may increase a person’s risk of heart disease. A major cause of heart disease is the buildup of fatty deposits in the walls of arteries over many years. The good news is there are things you can do to delay, lower, or possibly avoid or reverse your risk.
The most common aging change is increased stiffness of the large arteries, called arteriosclerosis (ahr-teer-ee-o-skluh-roh-sis), or hardening of the arteries. This causes high blood pressure, or hypertension, which becomes more common as we age.
High blood pressure and other risk factors, including advancing age, increase the risk of developing atherosclerosis (ath-uh-roh-skluh-roh-sis). Because there are several modifiable risk factors for atherosclerosis, it is not necessarily a normal part of aging. Plaque builds up inside the walls of your arteries and, over time, hardens and narrows your arteries, which limits the flow of oxygen-rich blood to your organs and other parts of your body. Oxygen and blood nutrients are supplied to the heart muscle through the coronary arteries. Heart disease develops when plaque builds up in the coronary arteries, reducing blood flow to your heart muscle. Over time, the heart muscle can become weakened and/or damaged, resulting in heart failure. Heart damage can be caused by heart attacks, long-standing hypertension and diabetes, and chronic heavy alcohol use.
Age can cause other changes to the heart. For example:
- There are age-related changes in the electrical system that can lead to arrhythmias—a rapid, slowed, or irregular heartbeat—and/or the need for a pacemaker. Valves—the one-way, door-like parts that open and close to control blood flow between the chambers of your heart—may become thicker and stiffer. Stiffer valves can limit the flow of blood out of the heart and become leaky, both of which can cause fluid to build up in the lungs or in the body (legs, feet, and abdomen).
- The chambers of your heart may increase in size. The heart wall thickens, so the amount of blood that a chamber can hold may decrease despite the increased overall heart size. The heart may fill more slowly. Long-standing hypertension is the main cause of increased thickness of the heart wall, which can increase the risk of atrial fibrillation, a common heart rhythm problem in older people.
- With increasing age, people become more sensitive to salt, which may cause an increase in blood pressure and/or ankle or foot swelling (edema).
Other factors, such as thyroid disease or chemotherapy, may also weaken the heart muscle. Things you can’t control, like your family history, might increase your risk of heart disease. But, leading a heart-healthy lifestyle might help you avoid or delay serious illness.
WHAT IS HEART DISEASE?
Heart disease is caused by atherosclerosis (ath-uh-roh-skluh-roh-sis), which is the buildup of fatty deposits, or plaques, in the walls of the coronary arteries over many years. The coronary arteries surround the outside of the heart and supply blood nutrients and oxygen to the heart muscle. When plaque builds up inside the arteries, there is less space for blood to flow normally and deliver oxygen to the heart. If the flow of blood to your heart is reduced by plaque buildup or is blocked if a plaque suddenly ruptures, it can cause angina (chest pain or discomfort) or a heart attack. When the heart muscle does not get enough oxygen and blood nutrients, the heart muscle cells will die (heart attack) and weaken the heart, diminishing its ability to pump blood to the rest of the body.
Find out more about heart attacks.
SIGNS OF HEART DISEASE
Early heart disease often doesn’t have symptoms or the symptoms may be barely noticeable. That’s why regular checkups with your doctor are important.
Contact your doctor right away if you feel any chest pain, pressure, or discomfort. However, chest pain is a less common sign of heart disease as it progresses, so be aware of other symptoms. Tell your doctor if you have:
- Pain, numbness, and/or tingling in the shoulders, arms, neck, jaw, or back
- Shortness of breath when active, at rest, or while lying flat
- Chest pain during physical activity that gets better when you rest
- Lightheadedness
- Dizziness
- Confusion
- Headaches
- Cold sweats
- Nausea/vomiting
- Tiredness or fatigue
- Swelling in the ankles, feet, legs, stomach, and/or neck
- Reduced ability to exercise or be physically active
- Problems doing your normal activities
Problems with arrhythmia are much more common in older adults than younger people. Arrhythmia needs to be treated. See a doctor if you feel a fluttering in your chest or have the feeling that your heart is skipping a beat or beating too hard, especially if you are weaker than usual, dizzy, tired, or get short of breath when active.
If you have any signs of heart disease, your doctor may send you to a cardiologist, a doctor who specializes in the heart.
WHAT CAN I DO TO PREVENT HEART DISEASE?
There are many steps you can take to keep your heart healthy.
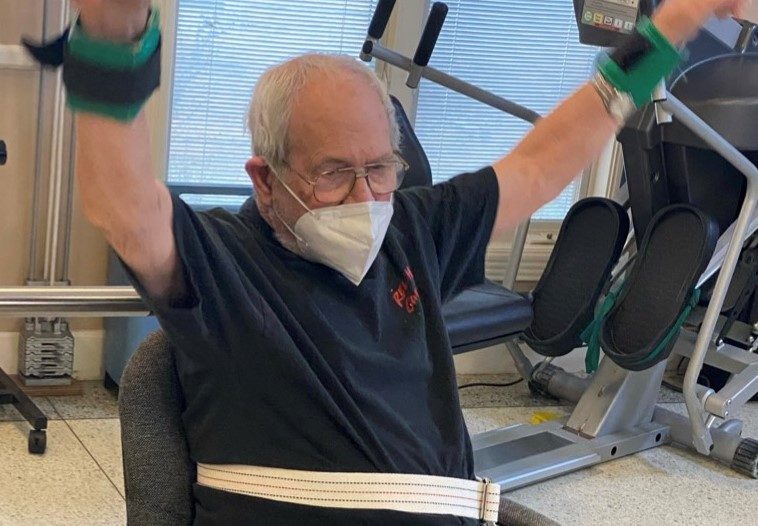
Try to be more physically active. Talk with your doctor about the type of activities that would be best for you. If possible, aim to get at least 150 minutes of physical activity each week. Every day is best. It doesn’t have to be done all at once.
Start by doing activities you enjoy—brisk walking, dancing, bowling, bicycling, or gardening, for example. Avoid spending hours every day sitting.
If you smoke, quit. Smoking is the leading cause of preventable death. Smoking adds to the damage to artery walls. It’s never too late to get some benefit from quitting smoking. Quitting, even in later life, can lower your risk of heart disease, stroke, and cancer over time.
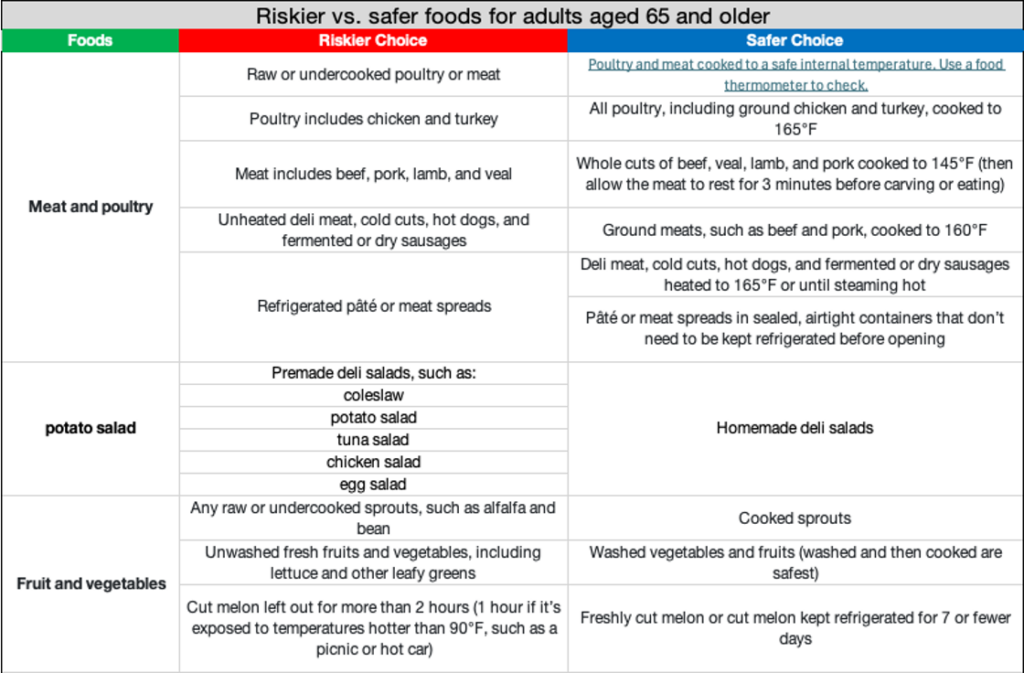
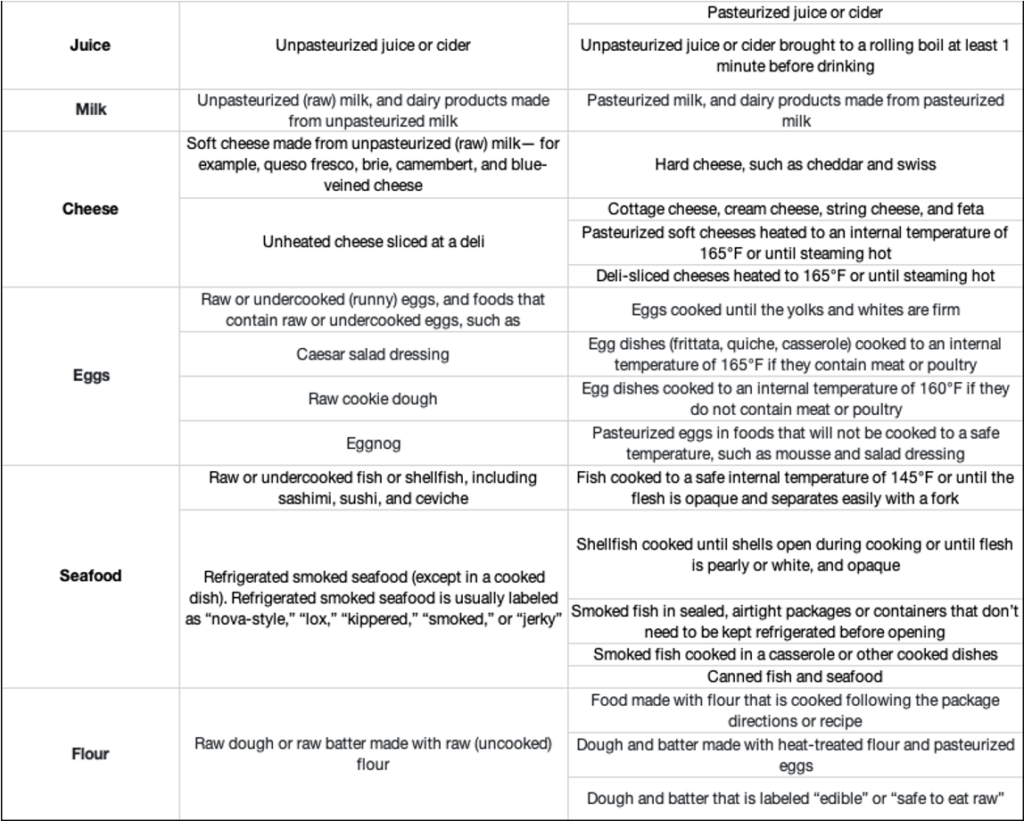
Follow a heart-healthy diet. Choose foods that are low in saturated fats, added sugars, and salt. As we get older, we become more sensitive to salt, which can cause swelling in the legs and feet. Eat plenty of fruits, vegetables, and foods high in fiber, like those made from whole grains. Get more information on healthy eating from NIA. You also can find information on the Dietary Approaches to Stop Hypertension (DASH) eating plan and the U.S. Department of Agriculture’s Food Patterns.
Keep a healthy weight. Balancing the calories you eat and drink with the calories burned by being physically active helps to maintain a healthy weight. Some ways you can maintain a healthy weight include limiting portion size and being physically active. Learn more about how to maintain a healthy weight from NIA.
Keep your diabetes, high blood pressure, and/or high cholesterol under control. Follow your doctor’s advice to manage these conditions, and take medications as directed.
Don’t drink a lot of alcohol. Men should not have more than two drinks a day and women only one. One drink is equal to:
- One 12-ounce can or bottle of regular beer, ale, or wine cooler
- One 8- or 9-ounce can or bottle of malt liquor
- One 5-ounce glass of red or white wine
- One 1.5-ounce shot glass of distilled spirits like gin, rum, tequila, vodka, or whiskey
Manage stress. Learn how to manage stress, relax, and cope with problems to improve physical and emotional health. Consider activities such as a stress management program, meditation, physical activity, and talking things out with friends or family. To learn more about stress management techniques, visit the National Center for Complementary and Integrative Health.
THE FUTURE OF RESEARCH ON AGING AND THE HEART
Adults age 65 and older are more likely than younger people to suffer from cardiovascular disease, which is problems with the heart, blood vessels, or both. Aging can cause changes in the heart and blood vessels that may increase a person’s risk of developing cardiovascular disease.
To understand how aging is linked to cardiovascular disease so that we can ultimately develop cures for this group of diseases, we need to first understand what is happening in the healthy but aging heart and blood vessels. This understanding has advanced dramatically in the past 30 years.
Today, more than ever, scientists understand what causes your blood vessels and heart to age and how your aging cardiovascular system leads to cardiovascular disease. In addition, they have pinpointed risk factors that increase the odds a person will develop cardiovascular disease. They are learning much more about how physical activity, diet, and other lifestyle factors influence the “rate of aging” in the healthy heart and arteries. The aging of other organ systems, including the muscles, kidneys, and lungs, also likely contributes to heart disease. Research is ongoing to unravel how these aging systems influence each other, which may reveal new targets for treatments.
In the future, interventions or treatments that slow accelerated aging of the heart and arteries in young and middle-aged people who seem to be healthy could prevent or delay the onset of heart disease, stroke, and other cardiovascular disorders in later life. Some interventions that we already know slow the rate of aging in the heart and arteries include healthy eating, exercise, reducing stress, and quitting smoking. The more we understand the changes that take place in cells and molecules during aging, for example, the closer we get to the possibility of designing drugs that target those changes. Gene therapies can also target specific cellular changes and could potentially be a way to intervene in the aging process. While waiting for these new therapies to be developed, you can still enjoy activities, like exercise and a healthy diet, that can benefit your heart.
To learn more, please visit https://www.nia.nih.gov/health/heart-health/heart-health-and-aging.